On-demand 3D printing of personalized human organs is still a scientific gleam in the eye, but researchers around the world continue to make significant advances in this and related fields. Just in the past week, we have learned of two bioprinting breakthroughs that could accelerate the advent of 3D-printed organs. Researchers in China claimed on Sunday, Oct. 25, to have developed the world's first blood-vessel bioprinter.
October 28, 2015
On-demand 3D printing of personalized human organs is still a scientific gleam in the eye, but researchers around the world continue to make significant advances in this and related fields. Just in the past week, we have learned of two bioprinting breakthroughs that could accelerate the advent of 3D-printed organs. Researchers in China claimed on Sunday, Oct. 25, to have developed the world's first blood-vessel bioprinter. And a couple of days earlier, Science profiled research being conducted at Carnegie Mellon University (Pittsburgh, PA) that enables 3D printing of soft biological materials by using a gel as a support structure during the additive formation process.
Chinese biotech company Sichuan Revotek Co. (Chengdu) says that it has developed a system composed of stem-cell-based bio-ink, which it calls Biosynsphere; a 3D bioprinter; and cloud computing platform that allows the fabrication of blood vessels, a vital step in the creation of personalized functioning organs.
Creating the necessary blood flow and vascular structure to supply organs with nutrients and oxygen is a fundamental challenge that has faced tissue engineers. "While the concepts of bioprinting are clear in terms of using 3D printers to facilitate the fabrication of live tissue and cellular structures with the goal being to stretch that toward organs, what has been truly challenging up until now is finding the tools and materials that can handle the job," writes 3DPrint.com, reporting on the technology. "From the software to the hardware and the actual ink, these are the areas those in research and development have reported lacking." And that is why this breakthrough research could have such a profound impact on the future of 3D-printed organs.
Further details on this research are scarce, however, although the company says that it is open to cooperating with international partners, according to Chinese news site Xinhua.
Researchers at Carnegie Mellon University (Pittsburgh, PA), meanwhile, have found a way to 3D print soft biological materials through an approach they call freeform reversible embedding of suspended hydrogels (FRESH). Team leader Adam Feinberg, a biomedical engineer, explained the process and its ramifications to Science reporter Nala Rogers in an article published on Oct. 23.
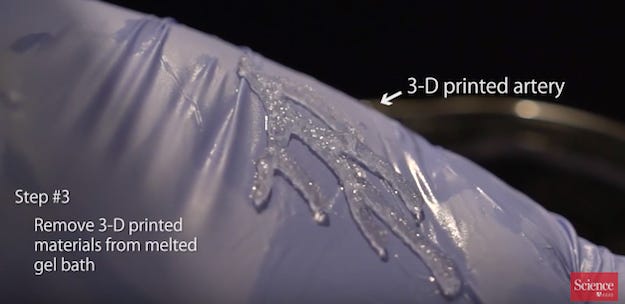
During the 3D-printing process, the biological objects are suspended in a slurry composed of blended collagen, which is semi-solid at room temperature. The slurry has a lower melting point than the printed part, and once the part has hardened into its final shape, the slurry is melted away. (Researchers at the University of Florida in Gainesville devised a similar system, notes Science, but the support gel is made of synthetic materials, which are washed off with water.)
"To put the FRESH system through its paces," writes Rogers, "Feinberg and his colleagues printed replicas of real organs based on magnetic resonance imaging and microscopy images." They printed a miniature human brain, scaled up heart of a baby chicken and an artery tree with walls that are less than 1 mm thick. The latter drew praise from a biomedical engineer at Cornell University, who is not involved in this project and is exploring a different method for 3D printing heart valves. "I don't know if we can make that geometry with our approach," Jonathan Butcher told Rogers. "The material complexity that they've been able to fabricate is really stunning."
The next step for Feinberg and his team is to incorporate live cells into the gel matrix. The researchers have already shown that cells can survive the FRESH process, reports Science, and they are now working on developing artificial heart muscle tissue, initially for drug testing but ultimately as a patch to repair damage from a heart attack.
A video about the research produced by Science is embedded below.
About the Author(s)
You May Also Like