Wireless brain sensors that incorporate bioresorbable electronics and materials have been developed by a team of neurosurgeons and engineers to temporarily monitor intracranial pressure and temperature. Once the implantable device is no longer needed, it is absorbed by the body, eliminating the need to surgically remove the device.
January 22, 2016
Wireless brain sensors that incorporate bioresorbable electronics and materials have been developed by a team of neurosurgeons and engineers to temporarily monitor intracranial pressure and temperature. Once the implantable device is no longer needed, it is absorbed by the body, eliminating the need to surgically remove the device.
Developed by scientists at Washington University School of Medicine in St. Louis and engineers at the University of Illinois at Urbana-Champaign, the resorbable implants potentially could be used to monitor patients with traumatic brain injuries, which kill approximately 50,000 people annually in the United States. Moreover, the technology could be applied to monitor activity in organ systems throughout the body. Their findings were published online on Jan. 18 in the journal Nature.
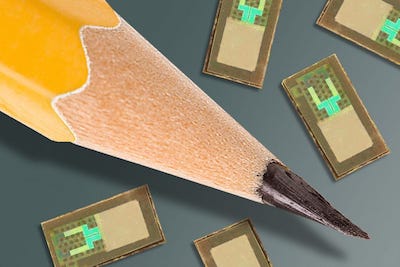
|
Image courtesy Washington University School of Medicine. |
"Electronic devices and their biomedical applications are advancing rapidly," said co-first author Rory K. J. Murphy, MD, a neurosurgery resident at Washington University School of Medicine and Barnes-Jewish Hospital in St. Louis. "But a major hurdle has been that implants placed in the body often trigger an immune response, which can be problematic for patients. The benefit of these new devices is that they dissolve over time, so you don't have something in the body for a long time period, increasing the risk of infection, chronic inflammation and even erosion through the skin or the organ in which it's placed. Plus, using resorbable devices negates the need for surgery to retrieve them, which further lessens the risk of infection and further complications."
The sensors build upon the pioneering work on "transient electronics" conducted by John Rogers and his team at the University of Illinois. They developed bioresorbable electronic devices based on very thin silicon sheets in the 20-nanometer range; water-soluble and biocompatible metals such as magnesium, zinc and titanium used as conducting components; and biologically based polymers that can be engineered to adjust the dissolution rate. "Rogers shunned fancy materials like graphene and used classic, cost-effective ones like silicone, instead. He simply played with the thickness and structure of these materials, so that rather than rigid, brittle wafers, he ended up with bendy, floppy sheets," writes Ed Yong in the Atlantic.
Rogers and Murphy refined this technology to produce a clinically usable pressure sensor consisting of a polylactic-co-glycolic acid membrane suspended in a frame of silicon and magnesium. "The pressure of the surrounding fluid causes the membrane to bend, which changes the electrical resistance of an adjoining silicon sensor," explains Yong in the article. "The whole device is then wrapped in a watertight polymer that gradually erodes over a few days, setting the lifetime of the sensor."
The sensors have been tested in baths of saline solution, which caused them to dissolve after a few days. Next, they were tested in the brains of laboratory rats. According to the researchers, the accuracy of the readings equaled current technology used in hospitals, which is essentially unchanged since the 1980s. "[The devices] are large, they're unwieldy, and they have wires that connect to monitors in the intensive care unit. They give accurate readings, and they help, but there are ways to make them better," says Murphy.
Having shown that the sensors are accurate and that they dissolve in the solution and in the brains of rats, the researchers now are planning to test the technology in patients.
"The ultimate strategy is to have a device that you can place in the brain—or in other organs in the body—that is entirely implanted, intimately connected with the organ you want to monitor and can transmit signals wirelessly to provide information on the health of that organ, allowing doctors to intervene if necessary to prevent bigger problems," Murphy said. "And then after the critical period that you actually want to monitor, it will dissolve away and disappear."
The National Institute of Mental Health of the National Institutes of Health, the Defense Advance Research Projects Agency and the Howard Hughes Medical Institute provided funding for this research.
About the Author(s)
You May Also Like